Assisted Procreation Treatments
Homologous and Heterologous of 1st and 2nd Level


Unfortunately, these are increasingly common issues today and they affect not only the physical aspect of the person involved but also the psychological one.
The center has long been dedicated to supporting couples in the challenging search for a pregnancy that is often long-awaited and desired.
The first step is to identify the specific causes that prevent conception and to implement therapies aimed at their treatment.
The diagnosis is made directly by the center's doctors following specific examinations. Where it has not been possible to heal the affected organ, based on the identified issue, the study of the most suitable assisted procreation treatments is undertaken.
CMR OFFERS VARIOUS TREATMENTS FOR MEDICALLY ASSISTED PROCREATION, BOTH HOMOLOGOUS AND HETERLOGOUS, OF 1ST AND 2ND LEVEL.

Today, there are various medications available for inducing ovulation, which are increasingly advanced and clinically effective, allowing for a highly personalized therapy to achieve the desired result.
An ultrasound monitoring will be associated to evaluate follicular growth starting from the 2nd-3rd day of the cycle.

IUI is the 1st level artificial fertilization treatment of assisted procreation (PMA) and involves moderate pharmacological stimulation of multiple ovulation. In some cases, it can be performed on a spontaneous cycle.
To monitor the progress of folliculogenesis, ultrasound checks and possible hormonal assays are required during the treatment.
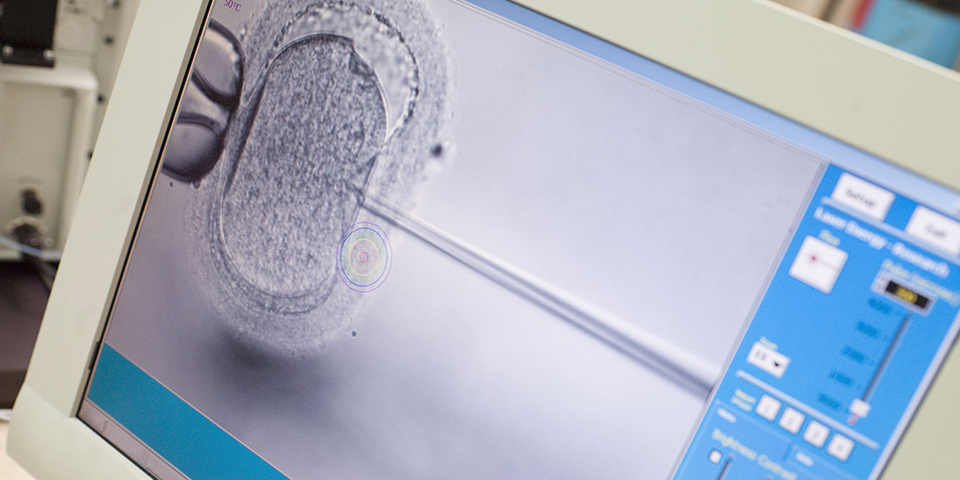
ICSI is a 2nd level assisted fertilization technique reserved for cases of severe semen abnormalities (very low sperm count and/or extremely reduced motility), or after failed fertilization of oocytes via IVF.
The procedure is similar to IVF except for the method of fertilizing the oocytes, which involves the introduction of a single spermatozoon, using a micro-needle connected to a micromanipulator and under microscopic vision, directly into the oocyte.

The CMR laboratory has been adopting this type of embryonic culture since 1998; it involves the culture of embryos in the laboratory extended until the 5th-6th day, when they reach the blastocyst stage, before transfer to the uterus.
The blastocyst stage is achievable in 90% of cases when there are at least 3 good-quality embryos after 48-72 hours from insemination, with results in terms of ongoing pregnancy exceeding 50%.

Heterologous fertilization represents the assisted reproductive treatment available to couples with irreversible sterility or infertility issues.
This treatment involves the use of assisted reproductive techniques, utilizing gametes (sperm, oocytes, or both) from an external donor.
Couples of different sexes with a diagnosis of infertility, whether married or cohabiting, where the woman is under 50 years of age, can pursue heterologous fertilization.
The Preimplantation Genetic Testing for Aneuploidies (PGT-A), previously known as PGS, allows for the evaluation of embryonic health status in all couples undergoing in vitro fertilization, even if they are not carriers of genetic diseases, enabling the transfer of embryos that genetic analysis shows to be free of chromosomal abnormalities.
This test combines the use of IVF techniques with the latest advancements in genetic research.
The Preimplantation Genetic Test for Monogenic Disorders (PGT-M), previously known as PGD, is a methodology that allows for the identification of genetic diseases or chromosomal alterations in embryos at very early stages of development, generated in vitro by couples at high reproductive risk, before their implantation in the uterus.
This test combines the use of IVF techniques with the latest advancements in genetic research.
The PGT-SR allows for the detection of structural chromosomal abnormalities caused by the incorrect breaking or joining of chromosomal segments, leading to the final result of a disease.
There are many types of structural alterations:
translocations, deletions, duplications, insertions, ring chromosomes, or inversions.
The PGT-SR represents an important tool in reproductive medicine, providing couples with the opportunity to increase their chances of having a healthy child.
Learn More
The vitrification of the patient's gametes and embryos is a laboratory procedure that preserves their characteristics over time.
Vitrification involves treating both gametes (when required) and embryos (in cases permitted by law) with cryoprotective substances and subsequently immersing them in liquid nitrogen at a temperature of -196° C; these very low temperatures keep the biological properties intact until thawing.
This procedure is far superior to older freezing processes, as it prevents the formation of ice crystals that could damage the cells.
It has been widely demonstrated by numerous studies that the survival rate after the vitrification process is approximately 97%.

The microfluidic selection of sperm is a method that uses a chip to mimic the natural environment of the female reproductive system. Through microchannels, sperm are selected based on characteristics such as morphology, DNA integrity, vitality, and motility, resulting in higher quality compared to unselected sperm.
This approach ensures high-quality selection, greater speed in the procedure, and a reduction in the risk of miscarriage and oxidative stress. It is particularly indicated for patients with high sperm DNA fragmentation, repeated IUI failures, low oocyte fertilization with ICSI, repeated miscarriages, and insufficient embryo quality.
Learn More
The staff at CMR is here to support you through the activation of an ONLINE CONSULTATION desk, where they will answer all your questions to establish a first approach and begin an important journey together.